Why do some endurance athletes have higher than normal HbA1c levels
Is your HbA1c higher than you think it should be?
I have spoken with many athletes and particularly endurance athletes have mentioned that their HbA1c numbers are higher than they think they should be and are continuing to creep up. Some of these athletes are starting to believe that they are becoming a borderline "pre-diabetic" with an HbA1c level of 5.7 to 6.3. How could this be happening? These are highly trained endurance athletes that eat well, are lean and very, very aerobically fit. They do full distance Triathlons, race 100 mile bike races and train intensely every week. What's going on?
I have been researching this now for 3 years and have found bits and pieces of different explanations, but nothing that definitely answers the question until a friend of mine, Joe Lavelle, who runs the Wise Athletes podcast sent me this article.
I can't begin to re-write or paraphrase this article in any meaningful or better way. It's just outstanding in every way. I will copy and paste their "Take Home" points below. Seriously, no one in 3 years has put this together, MAJOR kudos to Shriya Bakhshi. I highly recommend you read the entire article if you are interested in this stuff. It's excellent.
TAKE HOME POINTS
- Elite Endurance Athletes May Exhibit Elevated HbA1c Despite Exceptional Metabolic Health. While HbA1c is a trusted marker of average glucose over time, its interpretation can be misleading in elite endurance athletes. These individuals often exhibit low fasting glucose, high insulin sensitivity, and strong cardiovascular fitness, yet may present with HbA1c values in the 5.6–5.8% range—levels typically associated with prediabetes. This creates a diagnostic paradox: lab markers suggest impaired glycemic control in a population that routinely demonstrates superior metabolic regulation. Understanding this mismatch requires examining physiology beyond static lab thresholds.
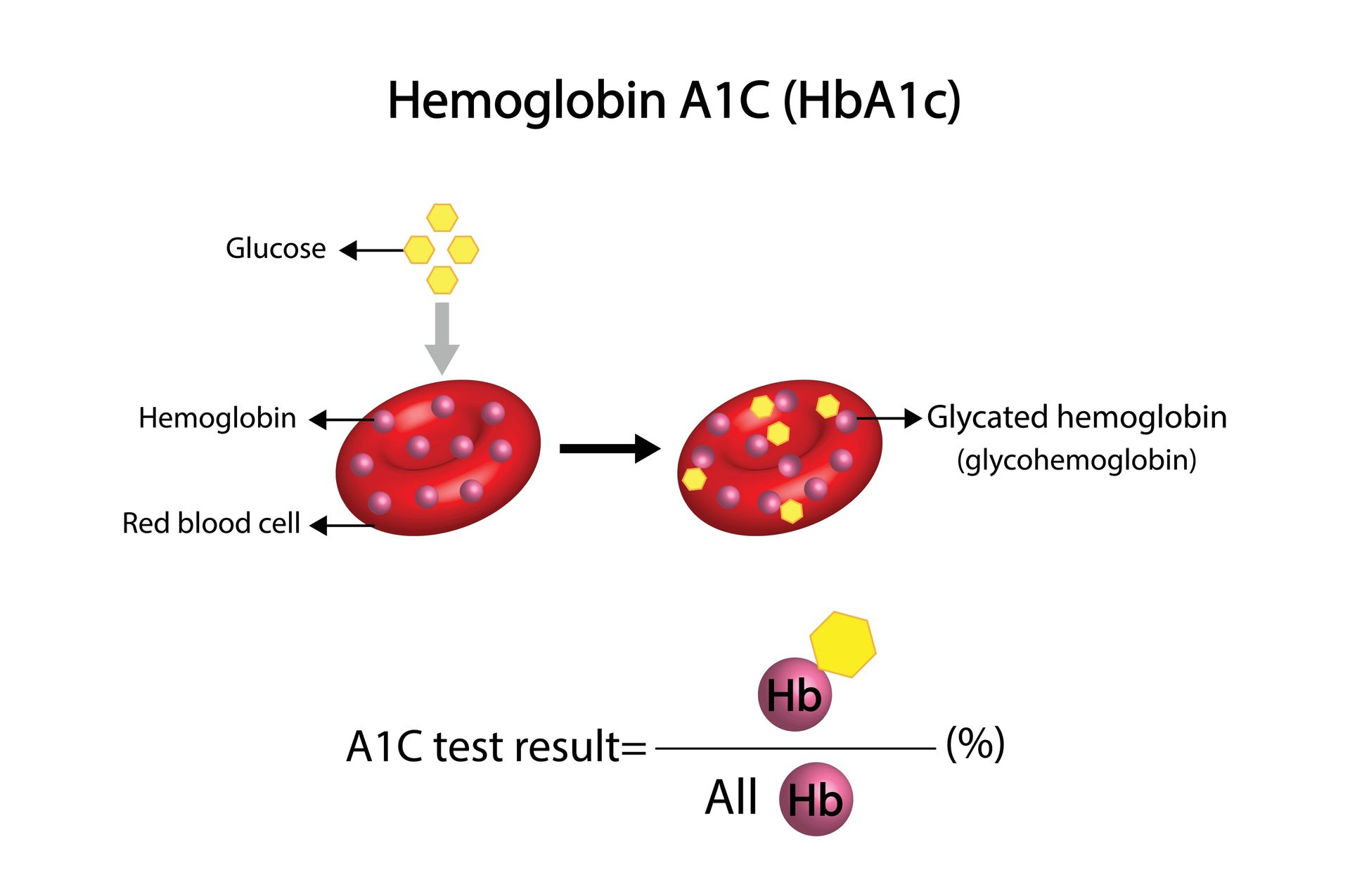
- Longer Red Blood Cell Lifespan in Athletes Can Artificially Elevate HbA1c. HbA1c reflects the glycation of hemoglobin over the lifespan of red blood cells, which is generally assumed to be ~120 days. However, chronic endurance training can subtly extend red blood cell lifespan by reducing oxidative stress, systemic inflammation, and mechanical damage. Studies suggest these cells may persist 10–20 days longer in well-trained athletes, increasing cumulative glycation exposure without an actual increase in blood glucose levels. This can nudge HbA1c upward in the absence of metabolic dysfunction, mimicking pathology where none exists.
- Cortisol and Catecholamines Can Raise Glucose Transiently—But Adaptively. Elite athletes experience frequent activation of the HPA axis during training, leading to elevated cortisol and catecholamine levels. These hormones promote glucose release through gluconeogenesis and glycogenolysis, prioritizing fuel availability for working muscles. In one study by Skoluda et al., hair cortisol concentrations in endurance athletes were significantly higher than in sedentary controls, reflecting chronic physiological stress. These repeated, adaptive glucose elevations may contribute to elevated HbA1c, even though they are performance-enhancing rather than pathological.
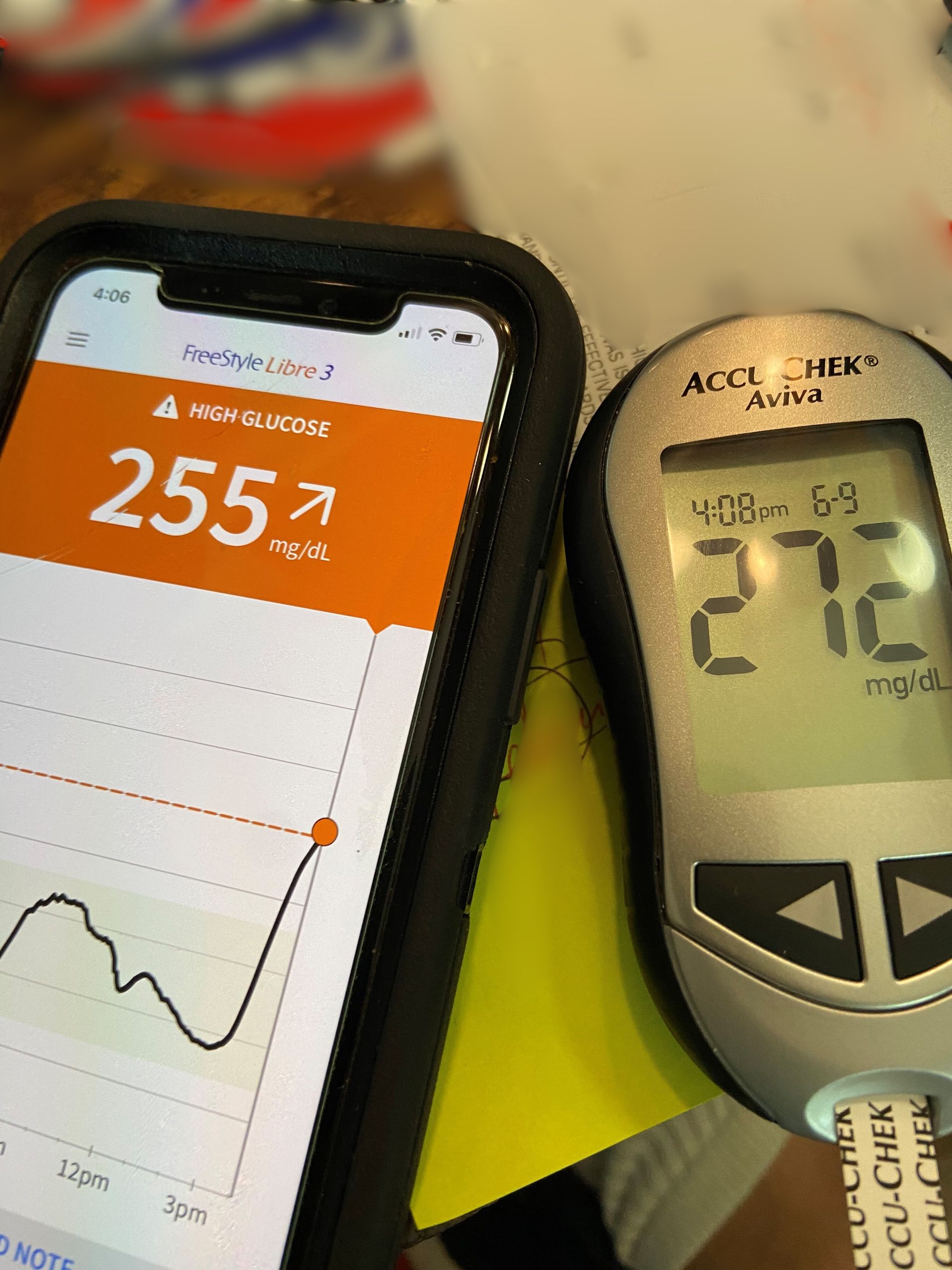
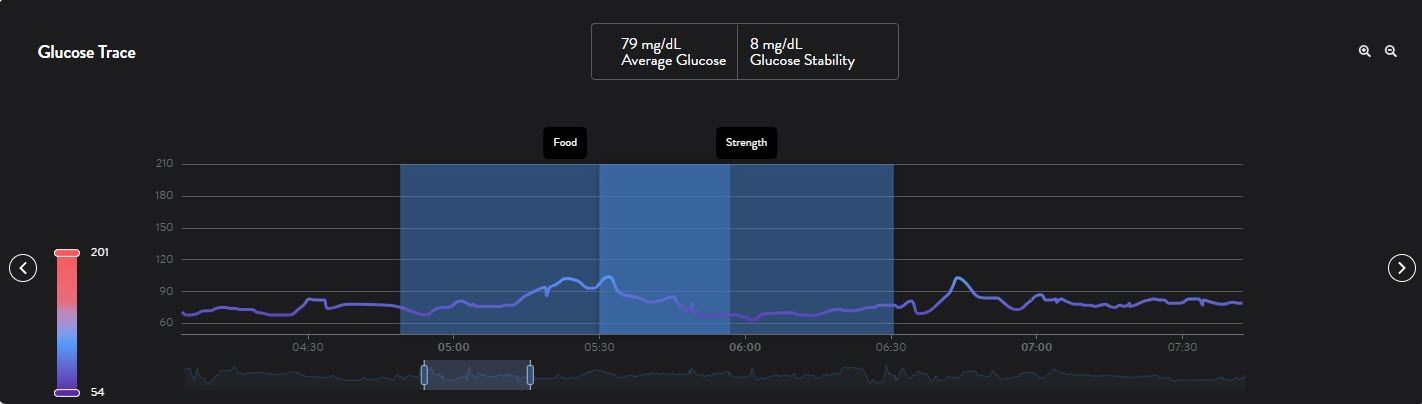
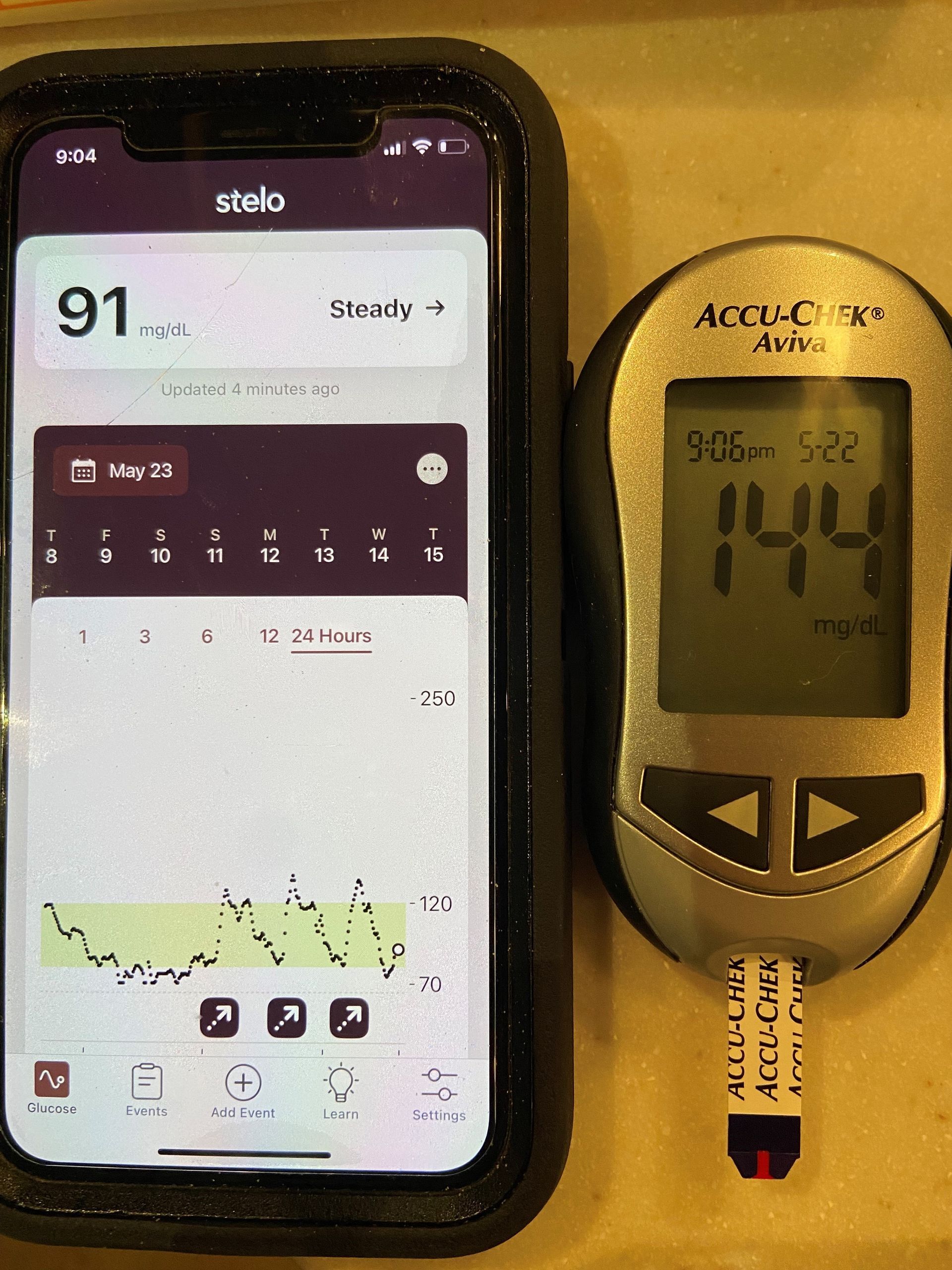
- CGM Data Reveal Transient Glucose Spikes and Dips Outside Normal Ranges. Continuous glucose monitoring (CGM) studies in elite endurance athletes show a wide glycemic range during training and recovery. Data from the Gatorade Sports Science Exchange reveal that these individuals can spend 10–20% of their day above 140 mg/dL and 5–7% below 70 mg/dL, even in the absence of insulin resistance. For example, professional soccer players have been observed exceeding 180 mg/dL during matches, while elite cyclists training at altitude averaged 108 mg/dL with peaks near 144 mg/dL. These fluctuations are adaptive responses to training, not signs of disease.
- Transient Insulin Resistance After Endurance Exercise Is Not Pathological. Following prolonged endurance activity, athletes may experience temporary reductions in insulin sensitivity, a phenomenon known as transient insulin resistance. A 2023 study demonstrated that after three hours of cycling at 65% VO₂max, athletes showed impaired glucose tolerance the following day on an oral glucose tolerance test (OGTT). Despite this, their resting OGTTs and fasting markers were normal. These temporary changes are part of the recovery and adaptation process and should not be mistaken for early metabolic disease.
- HbA1c Alone Is Insufficient for Assessing Glycemic Health in Athletes. Given the unique physiology of endurance-trained individuals, HbA1c should not be interpreted in isolation. Athletes with slightly elevated HbA1c may simultaneously exhibit fasting glucose in the 80–90 mg/dL range, low fasting insulin (<5 μU/mL), and low HOMA-IR scores—indicators of excellent glycemic control. When these metrics are considered together, they suggest a high-functioning metabolic system rather than early-stage insulin resistance. Dynamic testing, such as CGM or OGTT, provides a more accurate picture of glucose regulation in these populations.
- The “A1C Paradox” Is Not Limited to Professionals—Volume Matters. You don’t need to be an Olympian to experience this HbA1c shift. Recreational athletes who train frequently and at moderate to high intensities—such as marathoners, triathletes, and dedicated CrossFitters—can exhibit similar patterns. The determining factor is not elite status, but cumulative training load. Individuals who consistently exceed public health exercise guidelines (e.g., 150 minutes/week moderate or 75 minutes/week vigorous) may enter a physiological state where traditional glycemic markers become less reliable.
- Misclassification Has Real Consequences in Longevity and Biohacking Communities. As more health-conscious individuals adopt high-volume training as a strategy to improve healthspan, the risk of misclassifying adaptive physiology as disease increases. Mistaking a mildly elevated HbA1c for prediabetes may lead to unnecessary interventions—such as carbohydrate restriction, medication, or inappropriate dietary fear. Understanding the mechanisms behind the HbA1c paradox is essential for both clinicians and patients, ensuring that lab values are interpreted through the lens of training history, physiology, and function rather than one-size-fits-all reference ranges.